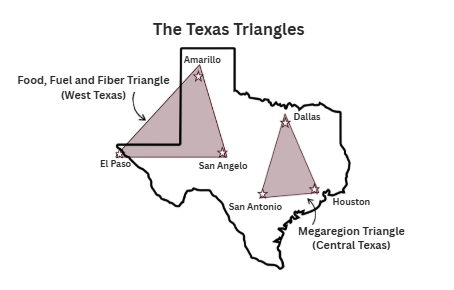
Health Care in the Texas Triangles
Third in a series on the Texas Triangles. Texas faces significant healthcare access disparities between its rural and urban communities. According to Health Care that Works for All Americans, rural Texans (roughly 16% of the state’s population) experience difficulty obtaining…



